- Health Blog
- Brochure Newsletter
- FAQ
- ACL Injury
- Back & Neck Care
- Bell’s Palsy
- Chronic Back Pain Management
- Frozen Shoulder
- Lower Back Conditions
- Managing Sports Injuries
- Neck Posture At Rest
- Pilates & Pregnancy
- Preserving Your Joints at Work
- Spine Health
- Strengthen Your Back For Sports
- Understanding Common Orthopaedic Conditions Among the 40's
- Work Your "Butt" Off
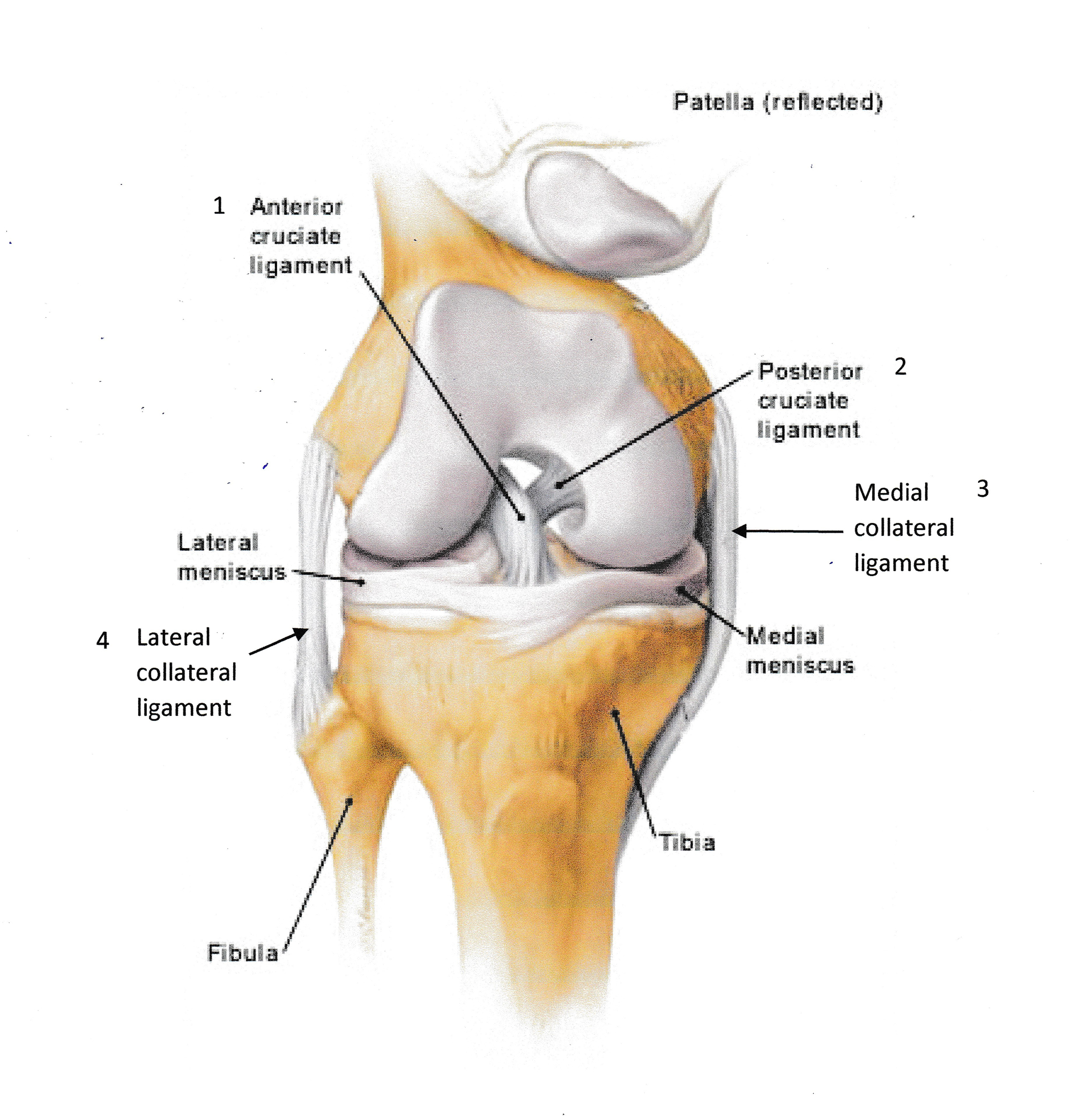
Anterior Cruciate Ligament (ACL) Injury
What is ACL?
There are 4 ligaments that supports the knee
1. ACL – anterior cruciate ligament (the cross ligament inside the knee joint)
2. PCL – posterior cruciate ligament (the cross ligament inside the knee joint)
3. MCL – medial collateral ligament (the outer ligament at the inside of the knee joint)
4. LCL – lateral collateral ligament (the outer ligament at the outside of the knee joint)
ACL is one of the 4 major ligaments that holds the knee. When it is strained or torn, it would affect the stability of the knee, giving rise to a sensation of “giving way”, “instability”, “swelling” and “pain”.
How do I know if I sustain an ACL injury?
ACL injury usually happens when the knee gave way after a jump from your land. However, you can also sustain ACL injury from hyperextension of the knee. With initial injury, there will be pain and swelling. An MRI can confirm if there is any ACL injury.
What should I do if I suspect I sustain an ACL injury?
You should consult an orthopaedic or sports doctor and get an MRI done. An MRI will be able to assess the severity of the tear and any associated injures to the meniscus and other knee ligaments.
What is the expected outcome of recovery?
Non-surgical repair – about 6 months, with physiotherapy. Surgical repair – full recovery varies between 5 months to 1 year, follow up with pre and post op physiotherapy.
What is Bell’s Palsy?
Bell’s Palsy is a medical condition in which the facial nerve becomes inflamed, swollen or compressed, thus, causing facial paralysis on one side of the face.
The facial nerve controls facial expression, eyelid movement and the muscles of the forehead and neck. As a result of the nerve injury, the patient has a drooling facial appearance. There is difficulty making facial expressions such as smiling, frowning, closing the eye. There is also difficulty eating and swallowing properly.
This condition is usually associated with viral infection affecting the facial nerves. It could happen to some patients a week or two after a cold, ear or eye infection.
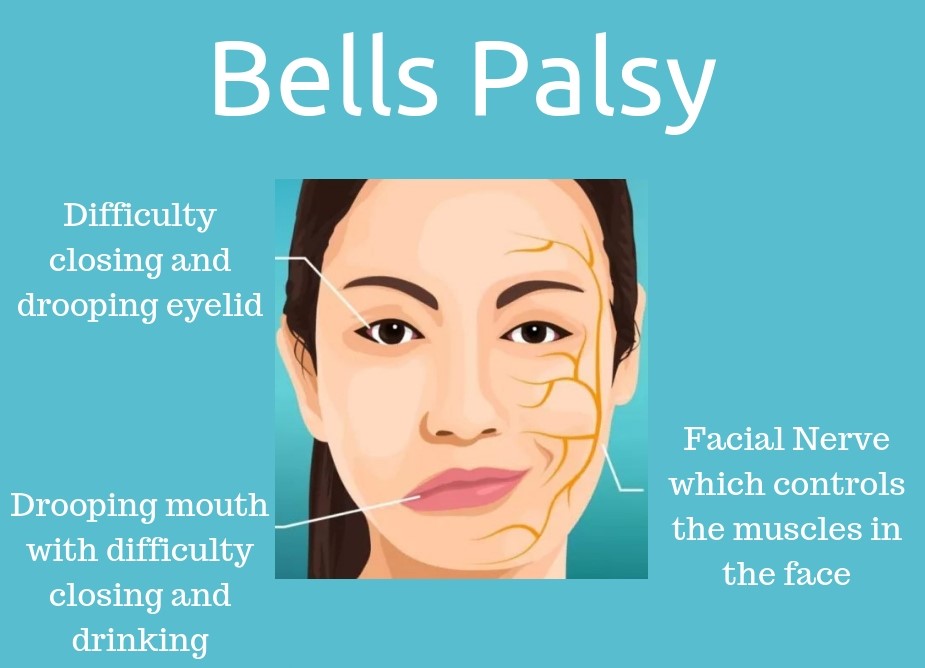
How do I know I have Bell’s palsy?
The symptoms come suddenly. You may wake up with facial drooling, difficulty swallowing and making facial expressions. When that happens, please don’t self-diagnose because a stroke or brain tumor may present with similar symptoms.
What do I do if I suspect I have Bell’s palsy?
Consult a family doctor and follow up with a physiotherapist. The doctor would prescribe medications and sends you for further investigation. A physiotherapist will use manual techniques and electrotherapy to stimulate the facial nerves to restore facial muscles function, prescribe exercises to improve your facial muscles control.
What is the expected outcome of recovery?
Time is the key for nerve recovery. Please seek treatment earlier for a better outcome and complete recovery. The time frame for a full recovery varies between 3 to 6 months, depending on the severity of damage to the facial nerves. In serve cases, some may have permanent damage.
Introduction
About 80% of us will experience back pain in our lives. Most people have the misunderstanding that only athletes or manual workers will suffer from back injuries. However, there is an increasing incidence of sedentary or desk bound office workers suffering from low back pain.
Most people recover from acute back pain within weeks. However, approximately 50% of these people who have had acute back pain develop chronic back pain i.e. pain lasting for more than 3 months. Many back pain sufferers shop around for doctors or alternative medicines to cure their back symptoms. But there is no magic cure. Up to today, chronic back pain management remains a challenge to healthcare professionals.
Muscle Dysfunction and Low Back Pain
The spinal column is the main structure that connects the arms and the legs. It works similar to the stem of a crane. When movement occurs at our arms or legs, the stem must be stable in order to perform safely and effectively.
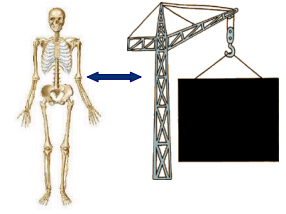
The stability of our spinal column depends on the ligaments, discs, bones and the deep trunk stabilising muscles, namely transversus and multifidus. Researchers have found that these deep trunk muscles weaken and fail to work effectively in patients with chronic low back pain.
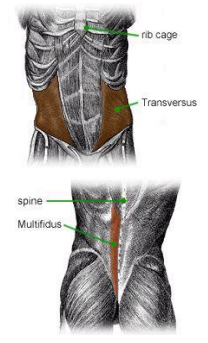
Faulty body movement has also been identified as a cause of long-term back problem. Muscle imbalance can develop after an injury or due to poor postures. Over time, the muscles in the back will become stiff and weak, forming thick bands. Most of us have it and we can feel it when we massage our back muscles. The circulation at these bands is poorer and this can give rise to muscle aches and pain. The weak and tight muscles also increase the stress at the spinal joints and discs, causing degeneration.
Various researchers say it is inappropriate to look at the spine in isolation. In the situation of chronic back pain, the musculature around the hips needs to be examined. Restrictions to the hip musculature are believed to induce excessive strain to the joints at our lower back. Therefore, in addition to the normal stretches to the back, stretches to the hip are as important.
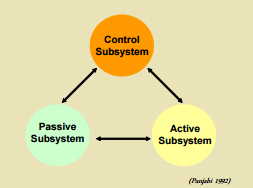
For successful management of chronic back pain, patients need to understand their conditions and take self-responsibility in the pain management. Panjabi (1992) proposed that spinal stability should be defined as the equilibrium of three subsystems: a) control subsystem - the ability of the brain to control the muscles and making it fire at the correct time; b) active subsystem - our muscles function; and c) passive subsystem - the bones, ligaments and discs. However, after an injury, there is usually a disturbance in these three systems.
Currently, the outcome of the attempts to manage these three systems is still unsatisfactory. This has been attributed to: patients’ lack of understanding of their conditions, lack of self-determination, lack of self-responsibility and motivation, poor compliance with exercises and inappropriate stretches and exercises prescribed.
Physiotherapy Management for Chronic Back Pain
Traditional physiotherapy management for chronic back pain involves analysis of body movement, prescribing stretches to the hips and back as well as prescribing core stabilizing exercises for the deep trunk stabilising muscles. Passive treatment like joint mobilisation (joint gliding motion), manipulation and massage may be prescribed based on assessment findings but this will be of a lesser focus because, as supported by current research, passive treatment is good only for short term relief but regular stretches and strength training are more crucial in preventing recurrence.
However, through experience, we realise there is more to traditional physiotherapy. We note that different body types respond differently to the same form of training. Managing chronic pain has to be more specific and may be different between individuals. There is always hope that the pain might disappear one day with proper training. This would require experienced personnel in identifying the cause of the physical problem and apply various training approaches in building the body system. Often, worksite evaluation and on field sports observation helps evaluate the effectiveness of treatment approaches prescribed and therefore, enhances the outcome of rehabilitation.
For successful management, the whole body system, including the mind and muscles, must integrate and work together to perform smooth and flowing motion. The patients need to learn movement awareness, be patient in changing faulty movement pattern and give time to build up their physique to cope with the daily activities in their lives.
Training mind-body connection and movement awareness, for example, using fundamental principles of Pilates; re-educating efficient movement pattern in daily activities and sports; incorporating strength training and postural correction are essential rehabilitation components that would create a longer lasting effect and improve the outcome of success.
Prevention is still the key to back pain management. Our body is made to move. Inactivity or lack of mobility to the joints can lead to early degeneration due to a lack of nutrition to maintain the healthy joints. Losing muscle mass is a process of ageing and this makes our body more prone to strains and sprains while we perform simple daily tasks. Therefore, participate in various form of exercise to let your body experience movement, to maintain muscle tone and stretch regularly. The importance of good posture cannot be emphasized enough. Above all, patients’ understanding of their conditions and self-motivation are the major determining factor to success.
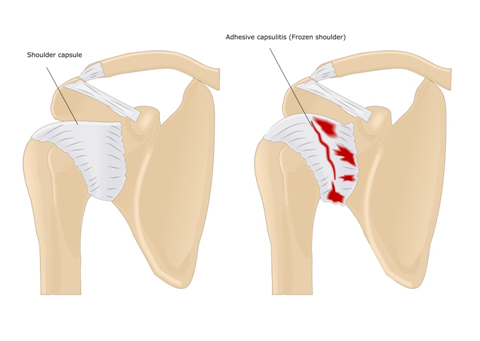
What is frozen shoulder?
Frozen shoulder in medical term is known as “adhesive capsulitis”. This is a painful condition of the shoulder capsule, which is a connective tissue that wraps around the shoulder joint. The shoulder capsule becomes inflamed and stiff, leading to a restriction in shoulder motion and pain.
How did it happen?
The cause is unknown. It is generally thought to be caused by an injury or trauma to the area and may have an autoimmune component.
Anyone over 40, who have poor posture and tend to round their shoulders forward, who have previous shoulder injury are prone to this condition.
How do I know I have frozen shoulder?
Patients with frozen shoulder usually notice that they have night pain while sleeping on their shoulder. The pain disturbs their sleep and it does not go away after weeks. Gradually, within the next 3 months, there is restrictions in shoulder motion.
They experience pain and difficulty lifting the arm up, scratching behind their backs, reaching behind their necks, reaching for their back pocket, and for ladies, hooking up their bras.
What do I do if I suspect I have frozen shoulder?
Consult an orthopaedic surgeon and follow up with a physiotherapist. An orthopaedic surgeon may prescribe medication or injection and sends you for further investigation.
Physiotherapists are medical professionals who teaches exercises and stretches to help you improve your medical condition. They use their trained hands to feel the tight muscles and release the tension in the muscles which causes restrictions to your movement. They apply electrotherapy to manage your pain.
What exercise should I do to help with frozen shoulder?
There are many exercises that you can do. But first consult a physiotherapist because exercises should be supervised.
Is swimming a good exercise for frozen shoulder?
Swimming is not advisable because if you try to exert on a painful shoulder, it may damage other structures as the body compensates due to pain.
What should I avoid doing?
Sleeping on the painful shoulder at night. Carry heavy things with the painful arm.
Will acupuncture help?
Acupuncture will help to reduce the inflammation at the shoulder and therefore, lessen the pain.
Will steroid injection help?
Steroid injection will help to reduce the inflammation at the shoulder and therefore, lessen the pain.
Will Platelet Rich Plasma (PRP) injection help?
PRP injection is rather new in the management of frozen shoulder but clinically, it has positive outcome in reducing pain for patients diagnosed with frozen shoulder.
What is the expected outcome of recovery?
The time frame for a full recovery varies between 6 months to 18 months. There will be initial pain and stiffness for about 6 months, followed by lesser pain but continuing shoulder stiffness for another 6 months. Then the stiffness will gradually ease. During this trying period, it is important to undergo deep tissue release, joint mobilization and stretches by a physiotherapist. Patients should also learn proper shoulder mechanics for a good outcome in recovery.
Recall your last overseas experience - how were the pillows in your room? Frequently, you find that the pillows provided at the accommodation are usually very soft. While it is fine for some people to sleep on softer pillow, others may experience morning neck pain and stiffness. If you are used to sleeping on a firmer pillow, here is a suggestion to overcome the problem:
- Roll up a towel and place it underneath the arch at your neck. The thickness of the rolled up towel varies from individual to individual because of different body type. You must feel that your neck is supported when you lie down on your back.
- Place the rolled up towel underneath the bottom edge of the pillow and above your shoulder level. Now, you are ready for a good night sleep!

The aim of a rolled up towel is to support the arch at your neck. It takes off the tension at the neck muscles when you are lying on your back. However, if you prefer to sleep on your side, then you would have to adjust the towel thickness accordingly while you are sleeping on your side. If you are unsure, please consult a physiotherapist.
Pregnancy is one of the most meaningful and remarkable experience in a woman’s life. Physical radiance, the surge of endorphins, and excitement about becoming a mother for the first time or again are among the most enjoyable benefits. However, pregnancy is also a physically and emotionally taxing experience because of the pain and discomfort arising from the anatomical changes. In fact, pregnant women typically develop lumbar lordosis (increased back arching), which contributes to a very high prevalence of lower-back pain, and it is pregnancy rather than childbirth itself that has the greatest effect on the pelvic-floor muscles, developing incontinence symptoms during this time.

Women with uncomplicated pregnancies should continue exercising at mild to moderate intensity levels to help offset some of these discomforts and to prepare for the birth ahead. Provided they receive clearance and special instructions from a physician, expectant mothers will benefit immensely from staying active throughout their pregnancy.
In clinical studies, it has been observed that people with a relatively flat lower back or those suffered from low back pain have poor activation of their buttock muscles. Those with knee pain usually fail to fire their gluteus medius sufficiently to stabilise their pelvis and knees, thus exaggerate dropped foot arches.
On the other hand, those who tend to stick out their buttocks excessively while walking or running have very tight buttock muscles. The tightness causes increase tension to the surrounding soft tissues (fascia) which could give rise to mid and lower back and knee pain.
Thus, “butt” work is one of the major focuses in minimising injuries. If your buttock muscles are tight, it is appropriate to stretch it out but if it is weak, then strengthening is the way to go. Here are some suggested strengthening exercises and stretches for buttock muscles. All exercises should be pain free. If you are not sure, please check with your doctors, physiotherapists, sports trainers or fitness instructors.
How Can Pilates Exercise Programs Help?
Pilates offer a mind-body approach that balances strength and flexibility training. It combines flexibility and strength training with body awareness, breathing and relaxation. Pilates exercise is perfectly suitable to preparing women for labour and a speedy recovery postpartum. A no-impact regime, it places special emphasis on restoring the spine’s natural curves (postural alignment) and on improving stability and mobility in the lumbar pelvic and shoulder girdles — all important factors during pregnancy and beyond.
1) Postural Alignment
Throughout the gestation period, postural alignment alters, and many muscles become imbalanced, which can put mechanical stress on the lower back, pelvis, hips and feet. The shoulders and upper back begin to round forward due to the increased weight in the chest, causing the chin and neck to poke forward, creating what is called a “forward head posture”. As a result, the mid and upper back muscles at the shoulder girdle become stretched and this can lead to neck and middle back ache.
The lower back develops a deeper arch due to increased weight at the womb, causing tightness and contributing to lower-back pain. Improving postural alignment is therefore a key benefit of Pilates training during pregnancy.
2) Lumbopelvic Region
As the baby grows, the woman’s center of gravity shifts, affecting coordination and balance. Pilates exercises can enhance these skills without compromising safety. In addition, the hormone relaxin affects the joints and connective-tissue collagen fibers in the pelvis, particularly the joints around the pelvis, namely the sacroiliac and symphysis pubis. Relaxin, while essential for the expulsion of the infant during birth, can produce the negative side effect of increasing instability in the pelvis. Strengthening the abdominals in a controlled and safe manner helps stabilize the lumbopelvic girdle.
3) Pelvic Floor and Incontinence
During pregnancy, your tummy muscles are stretched over your growing baby and may weaken as a result. Your pelvic floor muscles are also placed under great stress and tend to stretch and move lower down into the pelvis under the weight of the baby. As a result, you may find it harder to contract these muscles and to hold them for very long. If your pelvic floor muscles are very weak, you may find that you are leaking urine when you cough or sneeze. Pilates targets the tummy and pelvic floor muscles which is important for normal function and in sustaining quality lifestyle. Furthermore, many Pilates exercises are performed on a "hands and knees" position, and this is an ideal position for pregnancy. It helps to take a lot of stress off your back and pelvis.
4) Shoulder Girdle
The physical demands of lifting and carrying a newborn require upper-body strength and stability. A Pilates exercise program will strengthen the necessary muscles at the neck, shoulders and back.
Pilates Programs and Exercise Recommendations
Clients should be encouraged to take private Pilates lessons to ensure exercises are properly modified and adapted as the pregnancy progresses. At each trimester, there are different aims and objectives for the exercises program. For example,
1st Trimester – focus on general well being, stretching and general body toning. Exercising in lying down on the reformer and mat work are encouraged for relaxation and body stability.
2nd Trimester – focus on toning as the pregnancy has become more stable and fitness is important to sustain the pregnancy. Greater body changes are noticed as the body gain weight, with more fat deposits around the body.
3rd Trimester – focus on relaxation and more stretching. Exercises would need to be modified to a more upright position.
Questions and Answers
- How can Pilates help a mom-to-be prepare for labor?We educate the mother as to which muscles are required to work during labor and how to assess them. Then we strengthen those muscles and increase the muscle stamina so she can pace herself during labor.
- Will Pilates help avoid a postpartum flabby belly?Not always, but by getting the abdominal wall back in shape, it will help to reduce it.
- How often should a mom-to-be have a Pilates workout?It is best to start off two to three times a week. As the mom-to-be progresses through the pregnancy, the individual will determine how often they want to work out. Some lay off from Pilates 1 month before labour while others do Pilates till the day they deliver. It varies between individual as long as one is comfortable with their bodies.
- Can a mom new to working out start Pilates?Yes, of course, but they should find a teacher who has had a lot of experience with pregnancy and new moms. An established Pilates studio is strongly recommended rather than joining group classes which there is limited attention and supervision given. The teacher should be teaching for more than five years in a studio environment, because in a studio environment, there are more exposures and dealings with a variety of different bodies and other physical issues.
In some ways, our joints work similarly to a machine. In order to maintain healthy function, regular movement is important. Regular movement assists in the distribution of fluids within the joints and improve the nutritional supply to the cartilage.
You may say, “I move the whole day”. In actual fact, we seldom stretch our joints to its full range. Think about it: how often do you turn around fully to look behind your desk in the office? How often do you look up to the ceiling? Or stretch your arms back? Here are some tips to stretch out your lower back while at work. It needs to be done 5 times every hour.
While seated,
- Curl forward and bend down to touch the floor.
- Arch over to the side and bend sideways to touch the floor.
- Rotate and turn your trunk fully to look behind your left. Repeat it on the right.
- Slouch and sit up tall alternatively as in the picture.

- Take breaks, get up and walkabout every hour.
Do not jerk when performing any stretches. Think of the motion happening at each vertebrae. Move the spine in a controlled manner. As a precaution, if you have any history of back pain, please consult a physiotherapist before commencing these exercises.
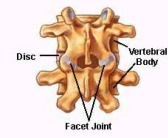
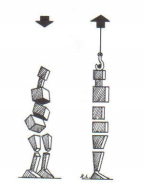
A normal spine comprises of 26 bones block and they stack up one on top of the other. These bones are held together by ligaments and muscles. As the shapes of the bones are not uniform, therefore, it gives rise to the 3 curves in our body.

Joints and Cartilage
The region where one bone is connected to another bone is known as “joint”. In healthy joints, the cartilage, which is the whitish coating covering the joint surface, is smooth. Its function is to reduce friction between the bones as they glide over one another.
Normal healthy joints are only well nourished through regular joint movement i.e. gliding over one another, compression and decompression. If you own an old car and did not start it every day, it will become inefficient and probably won’t run. The same goes for our joints. If we do not move it through full joint motion daily, the joint movement will become stiff and robotic rather than smooth and fluid. The cartilage can wear out due to disuse.
Sudden stretch to a stiff and compressed joint can produce “pop” sound (joint manipulation). Thus, popping joints is an indication of the condition of your joints.
Muscles
Muscles, on the other hand, need to contract and stretch to prevent it from getting tight and to maintain strength.
When the muscles are tight, blood and nutrients are unable to reach between the muscle fibres, causing it to be weak and ache easily. As a result, you may have heard of terms like “knots” in the muscles which are known as “trigger points”. Massage and heat therapy will usually help but they only provide temporary relief. This is because when we go back to our usual postures, the muscles will go back to its fixed pattern. Old habits die hard!
Tight muscles also compress on the underlying joints, causing the joints to become stiffer and harder to glide over one another.
Discs
Between the bone blocks, there is a soft gel cushion known as “disc”, whose function is to act as a shock absorber during walking, running, jumping and other weight loading activities. Our discs are like sponges that we placed between two hard objects. It becomes thin and wears out over time, leading to degeneration and reduced joint spaces.
You might have heard that we are taller in the morning and tends to be a little bit shorter towards the end of the day. That is because our body is usually lengthened in the morning, with good fluid content in our discs. As the day progresses, the fluid content decreases because of weight loading activities.
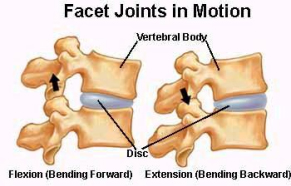
With all the stresses in life, lack of physical activity and effects of gravity, our bodies just give way to the downward force acting on our skeletal structure. Over time, our muscles become weaker and the joints and discs become compressed.
Postural Influence on Spine Structure, Muscles and Joints Development
It is without a doubt that uncorrected poor postures will contribute to all the pains and aches in your body. For example, we notice a flat tire when we look at our car and know that we need to pump it up; and we would adjust a picture that is hung crooked on the wall, but, how often do we look at ourselves in the mirror and notice that we are leaning off to one side; or throwing our hips forward; or rounding our shoulders; or letting go of our abdominals. We don’t do enough to change any part of ourselves that needs to be corrected. The reason is a lack of awareness and insight to the progressive deterioration leading to such poor body postures.
Why lengthening and spinal articulation?
Pilates talks about spinal articulation and lengthening of the spine. The principle behind lengthening is to increase the joint spaces so that the discs can stay healthy. Spinal articulation focuses on motion of every single bone, giving all the joints an opportunity to move, resulting in better joint nutrition and cartilage health.
About Us
We offer Pilates based exercise rehabilitation and movement education by combining the positive benefits of Pilates and exercise education to achieve optimal rehabilitation for acute and chronic spine pain.
Traditional strength and conditioning are also applied as different body types respond differently to the same training approaches, even with Pilates. For the best solution in managing physical health, contact us for an evaluation. Please call us at 63977397 / 82237914.
Myths and Misconceptions
- Only athletes are more prone to cartilage and joint degeneration. A sedentary lifestyle preserves our joints and cartilage. Understanding how the joints obtain its nutrition will help you understand that a sedentary lifestyle does not preserve cartilage and joint health. A lack of physical activity is not only bad for health but for the joints and muscles too! While athletes are more prone to injuries, and joint and cartilage degeneration, due to inappropriate training method and overtraining; there should be a balance in our physical activity level that allows our muscles to stretch and contract and our joints to move through a full range of motion. Selective exercises i.e. only exercising the legs and ignoring the upper body or vice versa may not be sufficient in looking after our body. Cross training and doing a variety of physical activities is more beneficial to improve physical coordination and balance.
- I feel good after cracking my spine. It gives me relief. Is it good to crack it every day?While self-manipulation may seem cool and make you feel good, a normal healthy joint should not crack. Joints that are degenerating and stiff tend to crack.
- It is unnatural and tiring to sit and stand up tall. Why should I bother about good posture? Think about stacking up 26 blocks in a slanted and disorganized manner, glue them together, and then give it 2 arms and 2 legs. Hang weight at the arms and bounce on the legs. That would be what happen to your spine without any active muscle control! Our bodies are made to move; muscles are made to work, to hold up the bones to perform purposeful and graceful movement. We should not take our body for granted.
- How can Pilates help?Pilates is a form of exercise that focuses on gaining awareness of your body and postures. The benefits of Pilates lie in incorporating the fundamental principles of breathing, spinal lengthening and abdominals control in toning, stretching and strengthening the muscles in your whole body. With the use of Pilates equipment, it helps improve the connection between your mind and your body to improve overall body coordination and balance. The body will then understand how to work as a unit to stabilize the various joints in the body including spine, shoulders, elbows, wrists, hips, knees and ankles.
- How do I get started on Pilates? Would it be beneficial to do Pilates group classes? What is a private one-on-one session? Depending on the quality and standard of the Pilates teacher, a group class setting may not be conducive or the best option to help you experience the maximum benefits of Pilates. A private session allows the Pilates instructor to assess your body structure and movement pattern so that a tailored program can be formed to help you achieve a greater benefit. To maximise outcome, a qualified and experienced Pilates teacher is the key!
Having a strong and stable trunk is an advantage no matter what sport you participate in. Strong trunk muscles provide a stable frame allowing our arms and legs to move more efficiently, thereby reducing the risk of injuries. A strong trunk also permits more efficient transfer of force between the upper and lower limbs. With efficiency, more power can be generated to enhance each serve, stroke or kick that is executed.

Traditional methods of back strengthening exercises include sit up, cross sit up, leg raises and back extension. Many athletes who develop the “6 pack”, that is the front abdominal muscles, are however unable to demonstrate co-ordinated spinal control. Recent researches support the importance of spinal stabilisation, focusing on the working of deeper trunk muscles. Over the years, Swiss ball exercises and Pilates have gained popularity as they involve exercises that target more than the superficial abdominal and back muscles. These exercises require the control of deep abdominal muscles and good mind-body coordination as well. With Swiss Ball activities, one must maintain a stable trunk during the execution of each movement, by keeping the ball as steady as possible without excessive hip movement. The key points to this exercise are to draw the belly button towards the back of the spine, tightening the muscles at the buttock, tightening and depressing the shoulder blades while maintaining a double chin.
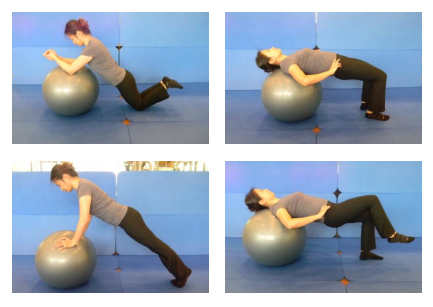
On the other hand, Pilates focuses on proper breathing technique, segmental control, articulation of the spine and flexibility. While core strength and stability is still the main focus, there is also more emphasis on segmental control of the spine (precision), flow of movement and centering (balancing on foot centres and strong pelvic floor). Proper breathing technique encourages more oxygen intake and promotes blood circulation. It also helps to “open up” the spine.

With proper training and feedback, one should transfer this control into functional tasks including standing, walking and sports activity. Deep core control has to be incorporated into daily activities, as it is not good enough to be able to do the exercises and activate the muscles only during Swiss ball exercises and Pilates. With the appropriate functional application into one’s activities of daily living, the risk of injuries can be minimised.
Apart from looking good and giving padding to our bones while seated, buttock muscles also contribute to the stabilisation of our back, knees and foot arches in upright motion. The three major muscles located at our buttocks are:
- Gluteus maximus
Assist one to get up from a seated position, to climb up stairs and slope.
- Gluteus medius
Essential in maintaining pelvic stability.
- Piriformis
Hip rotators and are usually found tight in people with back and hip pain. Tightness of this muscles lead to joint and nerve compression.
In clinical studies, it has been observed that people with a relatively flat lower back or those suffered from low back pain have poor activation of their buttock muscles. Those with knee pain usually fail to fire their gluteus medius sufficiently to stabilise their pelvis and knees, thus exaggerate dropped foot arches. On the other hand, those who tend to stick out their buttocks excessively while walking or running have very tight buttock muscles. The tightness causes increase tension to the surrounding soft tissues (fascia) which could give rise to mid and lower back and knee pain. Thus, “butt” work is one of the major focuses in minimising injuries. If your buttock muscles are tight, it is appropriate to stretch it out but if it is weak, then strengthening is the way to go. Here are some suggested strengthening exercises and stretches for buttock muscles. All exercises should be pain free. If you are not sure, please check with your doctors, physiotherapists, sports trainers or fitness instructors.
Strengthening the butt (10 sets of 10 daily)
1. Leg Lift to the Side
- Lie on your side, flex your feet, tighten the abdominals to firm up the waist line.
- Lift the leg up sideways by contracting the side butt muscles.
- Keep the knee cap facing forward as your lift up the leg.
- Keep the leg slightly back as you lift the leg up sideways.
- Lift and hold for 5 counts, then lower.

2. Side kick kneeling
- Kneel on your knees and then lean towards one side.
- Support yourself on the fist as in the picture.
- Lift the leg up sideways. Watch the posture in the final position, the legs form a 90 degrees right angle.
- Hold the leg up horizontally and sweep the leg smoothly forward and backward 10 times.
- Lower the leg for the next set.
- Repeat.

3. Body weight squat
- Stand with your feet at hip width apart.
- Lean your shoulder and trunk forward, stick back your buttock as though you are going to sit back on a chair to go into a squat position.
- A short cupboard as in the picture can teach you how to lean back with your buttock, without letting your knees come too far forward in front of the toes.
- Repeat.

Stretches
1. Self massage using tennis ball or trigger ball
- Place the ball under your buttock.
- Roll the ball in a circular motion to locate a sore spot at your buttock.
- Apply moderate pressure at the sore spot by sitting firmly on the ball.
- Gently roll the ball around the spot till pain eases (about 1 minute, 5 sets daily).

2. Knee to chest
- Lie down on your back.
- Support yourself on the fist as in the picture.
- Bring your knees as close to your chest as possible while keeping your butt on the mat.
- Hold for 30 counts, repeat 5 times daily.

3. Figure of 4 stretch
- Lie down on your back.
- Bring one ankle to the other knee as in the picture.
- Bring your knee towards your chest while keeping the buttock down on the mat.
- Feel the stretch at the side of your butt.
- Hold for 30 counts, repeat 5 times daily on each leg.

- Clinic Brochure
- Osteoarthritis Knee
- Squatting Exercises
- What is Physiotherapy? Physiotherapy is a healthcare profession that assesses, diagnoses, treats and prevents a wide range of health conditions and movement disorders. Physiotherapists are highly qualified and they work closely with orthopaedic surgeons, sports physicians, neurologists, cardiologists, GPs and other health clinicians to assist physical recovery and overcome disability through physical means such as manual therapy, soft tissue massage, electrical modalities and exercise rehabilitation. In addition, physiotherapy extends from health promotion to injury prevention, acute care, rehabilitation, maintenance of functional mobility, chronic disease management, patient and carer education and occupational health.
- How can physiotherapy help me?If you are suffering from any physical pain, such as neck or back pain, a physiotherapist would use manual technique or electrical modalities to cure your pain. A physiotherapist will also look into prevention of recurrence, prescribing exercises and stretches and advise you on adopting good body postures.
- If I have a neck or back or knee pain, should I see a chiropractor, physiotherapist or Chinese sinseh? In your best interest, you should see a physiotherapist first because a physiotherapist has the knowledge to diagnose, treat and advise you on further medical management. If you need to see a medical specialist for further investigation, they can advise and refer you appropriately.
- What happen if I pull my muscle while working out in a gym?Consult a doctor and get some anti-inflammatory medication. Apply ice to the injured area for 15 minutes 4 times a day for the first 2 days. Avoid drinking alcohol and applying heat to the injured region in the first 2 days. Consult a physiotherapist for a speedy recovery.
- Which is a better form of exercise for me if I have a back pain – Pilates or Yoga? Pilates originates as a rehabilitation tool for the injured soldiers back in the Second World War. Pilates increases flexibility as well as build core muscle strength and improve body awareness, all of which will help alleviate low back pain. Yoga does not originate as a rehabilitation tool. For those with low back pain due to weak muscles, spinal instability and spinal degeneration, Pilates equipment work would be more beneficial. For those who are generally stiffer in their joints and muscles, yoga would help at the beginning phase.
- How is Pilates and Yoga different?Pilates and Yoga are two different systems, each with its distinctive origin, philosophy and methods of practice.
a) ROOTS OF ORIGIN
Yoga has its roots in religion whereas Pilates has its roots in physical rehabilitation.
b) PHILOSOPHY
Yoga is more for those who want to improve body flexibility, do muscle toning and meditation whereas Pilates is more for people who have goals about changing their bodies seriously. Pilates originates as a form of rehabilitation back in the Second World War for injured soldiers. Up to today, Pilates is still a tool which is used for rehabilitation of the back and other spinal problems, knee problems etc. Yoga does not originate from rehabilitation of the body and has never been. Pilates is more scientific in improving the body conditions.
c) METHODS OF PRACTICE
i) Breathing
Yoga uses abdominal breathing i.e. abdominal rises as a result of inhalation. Pilates, on the other hand, involve abdominal bracing and you are not supposed to see the rising and sinking of the abdominal wall as you breathe. In Pilates, movement comes from the center or deeper abdominals, called “Powerhouse”. During respiration, the abdominals and back muscles contract to brace the trunk so as to encourage greater chest expansion. As a result, there is more oxygenation of blood to the body, thereby bringing about good health and healing.
ii) Physical Postures
Yoga focuses on many stationary poses and one is required to stay in the “asanas” for some duration for meditation. In Pilates, movement flows from one exercise piece to another and there is no holding of physical postures. In Pilates, the focus is on the quality rather than quantity of movement, constantly moving from one point to another with only a few repetitions of each movement piece.
iii) Precision In Movement
In Pilates, each movement piece can be broken down and there are stages in progression to the final movement piece. The levels of progression are meant to prepare the body physically for the demand required in each movement piece. Principles of spinal lengthening, spinal articulation, and movement initiated from the core muscles are main essences to the Pilates movement. For individuals who are unable to perform due to musculoskeletal issues e.g. muscle and joint stiffness, injuries etc, this is very useful. In Yoga, it is not specific into how you stretch your body, there is no one way to get to the final “asanas”.
iv) Eyes
In Pilates work, it requires mental concentration and the eyes are opened, gazing with purpose. This is usually not a focus in any other form of exercise.
v) Use of Equipment or Machines
In addition to exercises performed on a mat, Pilates uses equipment including Reformer, Trapeze Table, Wunda Chair, Spine Corrector etc to achieve spinal elongation and articulation, muscle lengthening, joint release and muscle toning. This is a method practised by many in the rehabilitation field as a tool for body conditioning and toning as our body works better when our hands and feet are in contact with an object (closed kinetic chain).


